Acute Red Eye
A red eye is the most common ocular disorder that primary care physicians encounter. Most cases are
relatively benign. Some, however, herald a vision-threatening or even life-threatening disorder. A detailed
description of the full differential diagnosis of a red eye is available elsewhere.1 This overview does
not assume that the examiner has access to a slit lamp or has been trained to use it.
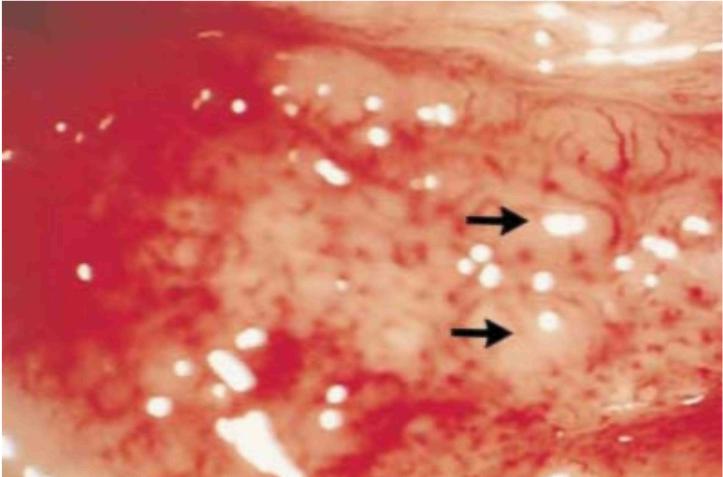
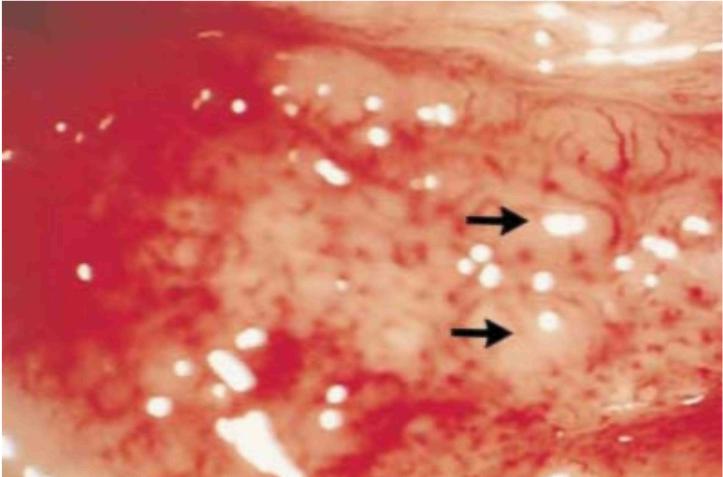
A subconjunctival hemorrhage (Fig. 1) is often the cause of acute ocular redness.The diagnosis is
based on simple observation of the characteristic features of such a hemorrhage: the redness, which is unilateral,
is localized and sharply circumscribed, the underlying sclera is not visible, the adjacent conjunctiva is free of
inflammation, and there is no discharge. There is also no pain, and vision is unaffected. Contributory factors
include trauma (which may be so minor that the patient does not recall it), fragile conjunctival vessels, bleeding
disorders, anticoagulation therapy, and hypertension. A subconjunctival hemorrhage sometimes results from prolonged
coughing, vomiting, or a vigorous Valsalva maneuver. No specific treatment is necessary, but an evaluation for con-
tributory factors should be undertaken. The patient should be reassured that the hemorrhage will clear gradually in
two to three weeks. Failure to resolve suggests a less common cause (e.g., Kaposi's sarcoma) and warrants a
referral to an ophthalmologist.
Of the disorders that cause a red eye, conjunctivitis is the one that the primary care physician is
most likely to encounter.2-5 Conjunctivitis is characterized by dilatation of the superficial
conjunctival blood vessels, resulting in hyperemia and edema of the conjunctiva, with discharge. A purulent
discharge generally suggests a bacterial infection, but otherwise, the nature of the discharge is not clinically
useful in determining the cause. Fluid may accumulate beneath the loosely attached bulbar conjunctiva, causing it to
balloon away from the globe (a phenomenon known as chemosis). Patients with conjunctivitis do not usually report
visual problems or ocular discomfort.
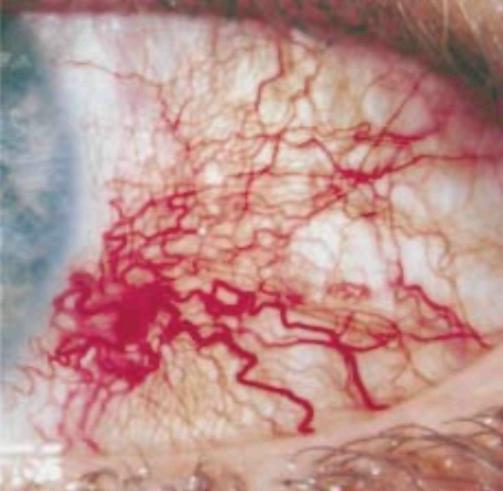
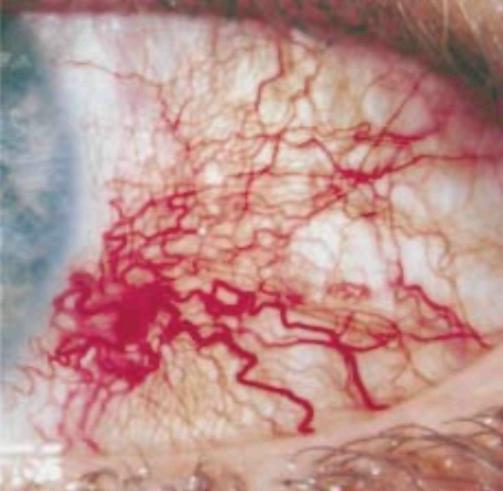
Conjunctivitis due to viral infection (Fig. 2), the leading cause of a red eye, is characterized by
conjunctival hyperemia and edema, a watery discharge, and occasionally small hemorrhages. The disorder often affects
one eye first and the other a few days later. The lids may be swollen. Conjunctivitis may develop during or after an
upper respiratory tract infection or after exposure to a person with such an infection. A watery discharge may cause
intermittent blurring, but vision is otherwise unaffected. Photophobia is uncommon. A palpable preauricular lymph
node strongly supports the diagnosis but is not present in the majority of cases. Viral conjunctivitis is usually
self-limited, but there is evidence that treatment with a topical antibiotic shortens its course.6
Broad-spectrum antibacterial eye-drops (e.g., a combination of trimethoprim [1 mg per milliliter] and polymyxin B
[10,000 units per milliliter], one or two drops four times a day) are often prescribed. The ostensible reason for
this treatment is to prevent bacterial superinfection, but the actual reason in many cases is that the patient will
not accept a recommendation that no therapy be administered. Topical antiviral drugs are not
administered.7 The patient must be informed that viral conjunctivitis is highly contagious. In cases of
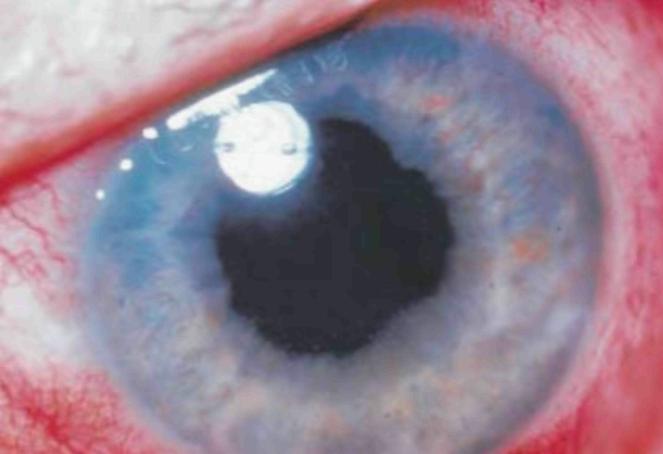
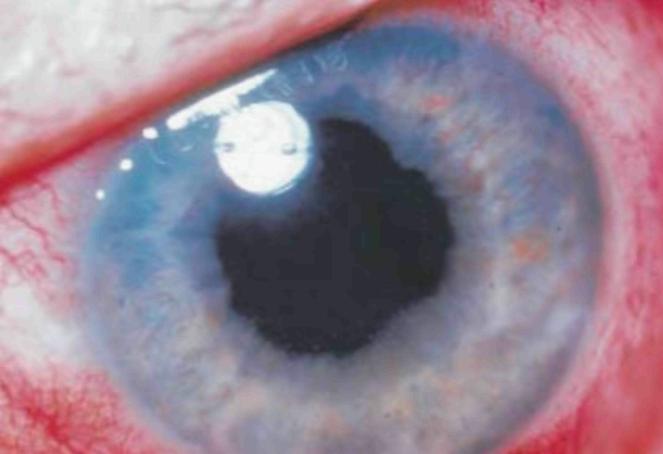
adenoviral conjunctivitis (Fig. 3) and presumably other forms of viral conjunctivitis, replicating virus is present
in 95 percent of patients 10 days after the appearance of symptoms but in only 5 percent on the 16th
day.8 The patient should be told not to share towels or other objects that might be contaminated and to
avoid close contact with other persons, including indirect contact (e.g., in a swimming pool), for approximately two
weeks. Similarly, the physician must be thorough with hand washing and decontamination of instruments.9
If there is no improvement in 7 to 10 days, the patient should be referred to an ophthalmologist.
Bacterial conjunctivitis is caused by a wide range of gram-positive and gram-negative organisms,
but the former predominate.10 Acute bacterial conjunctivitis typically has an abrupt onset, develops in
one eye initially but spreads to the opposite eye within 48 hours, and is manifested as tearing and ocular
irritation at the outset. A mucopurulent or purulent discharge develops within one or two days, with a collection of
debris at the base of the lashes and matting of the lids, particularly on awakening. Examination reveals diffuse
hyperemia of the bulbar and tarsal conjunctiva, generally without marked lymphadenopathy, though in unusual cases
(e.g., those associated with cat-scratch fever or tularemia), a preauricular or submandibular lymph node may be
palpable. In most cases of bacterial conjunctivitis, the diagnosis and the identification of the presumed pathogen
are based on clinical evaluation. Laboratory studies are performed to identify the organism and determine its
sensitivity to antibiotic agents only in severe cases and those that are unresponsive to initial treatment.


Treatment consists of a broad-spectrum topical antibiotic administered four times daily. This
empirical approach is highly effective, and adverse consequences are infrequent.6,10-12 The preference is
a 7-to-10-day course of gentamicin (0.3 percent) or tobramycin (0.3 percent) eyedrops. Though also highly effective
and still widely used in the United Kingdom,5,13-15 topical chloramphenicol (0.5 percent) has been
associated with a rare but devastating aplastic anemia 16-18 and is not used routinely in the United
States. The topical fluoroquinolones ciprofloxacin (0.3 percent) and ofloxacin (0.3 percent) are also highly
effective10-12 but should be reserved for severe infections. Bacitracin (500 units per gram) and
erythromycin (0.5 percent), which are effective against gram-positive bacteria, are available only in the form of
ointments that are difficult to instill and that blur vision. Oral antibiotics alone may be insufficient to treat
bacterial conjunctivitis in adults.19 If the disorder does not improve in one week, the patient should be
referred to an ophthalmologist.

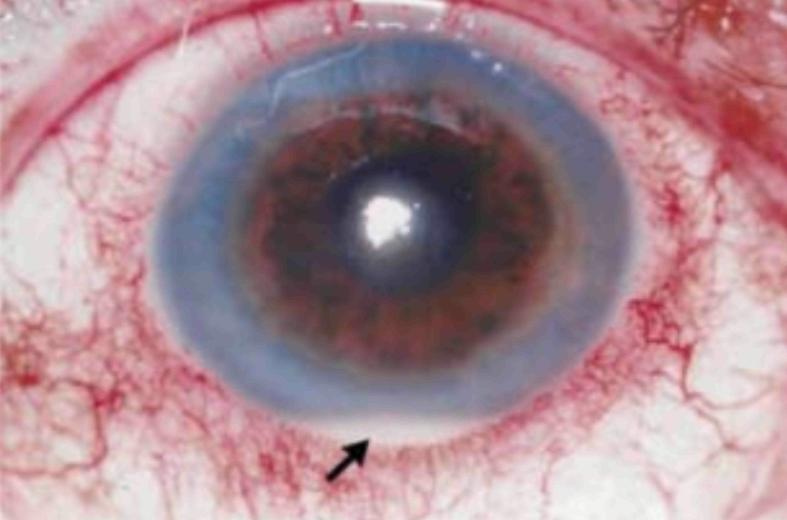
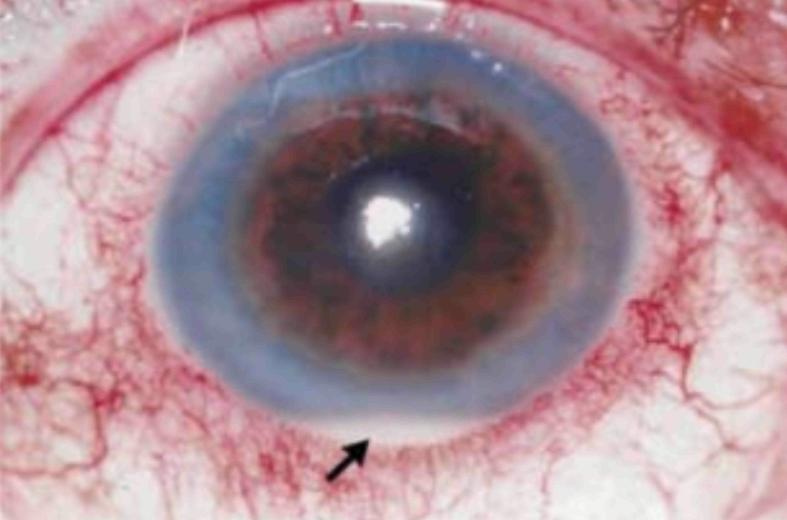
Hyperacute bacterial conjunctivitis (Fig. 4), characterized by an abrupt onset, a copious purulent
discharge, and rapid progression, is usually associated with a gonococcal infection in a sexually active adolescent
or adult. The conjunctiva becomes bright red and chemotic, and an inflammatory membrane (consisting predominantly of
leukocytes and fibrin) may develop on the tarsal conjunctival surface. The abundant discharge usually reaccumulates
rapidly after it has been wiped away. Preauricular adenopathy is often present, and there is marked

swelling of the lids, with aching and tenderness on palpation. Because of the abrupt onset of this
disorder and the severity of the signs and symptoms, the patient often seeks care before the infection affects both
eyes.
Hyperacute conjunctivitis requires aggressive treatment; if left untreated, the infection may involve the cornea,
rapidly causing peripheral ulceration and ultimately leading to perforation.21 Immediate referral to
an ophthalmologist is indicated. Treatment with topical antibiotics (bacitracin, erythromycin, or ciprofloxacin)
plus a full systemic regimen with an antibiotic against gonorrhea should be instituted immediately. Treatment of
gonococcal conjunctivitis with a single 1-g dose of intramuscular ceftriaxone has been effective.22
Because gonococcal conjunctivitis is a venereal disorder, the patient should be asked about symptoms of
urethritis and vaginitis (if the patient is female) and about sexual contact with persons who might be infected.
Chlamydial infection causes trachoma and the adult and neonatal forms of inclusion conjunctivitis.
Trachoma that results in blindness, one of the most common diseases in humans, is seen only sporadically in the
United States. Fortunately, neither adult nor neonatal inclusion conjunctivitis causes loss of vision, unlike
endemic trachoma.
Inclusion conjunctivitis in adults and adolescents (Fig. 5) is a sexually transmitted disease that
is common in urban areas. The disorder is almost always acquired through exposure to infected genital tract
secretions, transmitted from hand to eye or from genitalia to eye. The associated genital tract infection is usually
asymptomatic, but male patients may have symptomatic urethritis, and female patients may have chronic vaginal
discharge.
23
Symptoms and signs of inclusion conjunctivitis may be acute or subacute in onset and are often unilateral
initially. The patient generally has a red, mildly irritated eye, with a mucopurulent or purulent discharge and
lids that are stuck together on awakening. A preauricular node is frequently present on the affected side. There
is generally no history of fever or upper respiratory tract infection. A follicular response, most marked in the
inferior conjunctival fornix, may be apparent with the use of a magnifying device. Scarring of the conjunctiva,
which is characteristic of trachoma, is rarely present in adolescents or adults with inclusion
conjunctivitis.23
Oral treatment with tetracycline or erythromycin (250 mg four times a day) or doxycycline (100 mg twice a day)
for 14 days is required to eradicate inclusion conjunctivitis in adults and adolescents.23 Cure rates
exceed 95 percent.24 Topical therapy may suppress the ocular symptoms temporarily but does not affect
the genital reservoir of the disease and is therefore not effective when used alone. Treatment of sexual
partners helps prevent reinfection. Since tetracycline cross the placenta and may be deposited in the deciduous
teeth of offspring, they should not be given to pregnant women.25 Tetracyclines can also cause
lifelong discoloration of the permanent teeth if given to patients who are less than eight years
old.26 Chlamydial infection is managed with erythromycin in such patients.
Seasonal allergic conjunctivitis, a type I, IgE-mediated hypersensitivity to pollen, animal dander,
or dust, is the most common form of ocular allergy and is often encountered in patients with atopic
disease.
27 Perennial allergic conjunctivitis is similar, but the symptoms are less severe. Conjunctivitis
medicamentosa, a contact allergy, is characterized by a red eye with eyelid edema, erythema, and scaling in a
patient using a topical ophthalmic medication. The hallmark of allergic conjunctivitis is itching, often accompanied
by tearing and nasal congestion. There is bilateral dilatation of the conjunctival blood vessels, with varying
degrees of chemosis and a mucoid discharge.
Removing the offending allergen when possible or diluting it by instilling artificial tears is a simple,
effective treatment. Conjunctivitis medicamentosa can be treated simply by discontinuing the medication that
causes the allergic reaction. Topical and systemic antihistamines relieve itching; the choice of a topical agent
is levocabastine hydrochloride (0.05 percent four times a day). Over-the-counter eyedrops that contain an
antihistamine (antazoline or pheniramine) combined with a vasoconstrictor (naphazoline hydrochloride) can be
effective in mild cases. These preparations relieve itching and whiten the eye by constricting the conjunctival
blood vessels, but they can cause a reactive hyperemia with prolonged use.28 Although topical
mast-cell stabilizers (cromolyn sodium [4 percent] and lodoxamide tromethamine [0.1 percent]) can be used, the
clinical response is not immediate. These drugs must be given for approximately two weeks to prevent the release
of histamine and other chemotactic factors. Treatment with topical non-steroidal antiinflammatory drugs has
variable results.
Blepharitis, an acute or chronic inflammation of the eyelid often associated with conjunctival
inflammation, is caused by a variety of infectious agents, allergic disorders, and dermatologic diseases. When
bacteria, particularly staphylococci, colonize the eyelash follicles and the meibomian glands, excess secretion of
abnormal lipids occurs.
29,30 Ocular irritation ensues, with sensation of the presence of a foreign body,
accompanied by erythema and edema of the eyelid margins, misdirection and loss of eyelashes, conjunctival hyperemia,
and instability of the preocular tear film.
31,32 The resultant drying of the corneal surfaces exacerbates
the conjunctival hyperemia and causes microscopic erosions of the corneal epithelium, mild visual distortion, and
photophobia. Since most cases are chronic and require long-term therapy, they are best managed by an
ophthalmologist.
Abnormal apposition of the eyelid margins to the globe can cause a red eye. Entropion (inward rotation of the
margin of the eyelid) and trichiasis (misdirection of the lashes toward the cornea) can irritate and abrade the
ocular surface. Ectropion (outward rotation of the margin of the eyelid) can cause anomalous spreading of tears
over the ocular surface; exposure keratopathy (excess evaporation of tears and drying of the corneal surface)
may ensue if the eyelid abnormality is severe. Entropion and ectropion can usually be diagnosed by inspecting
the eyelid. Since definitive treatment frequently requires surgical intervention, patients with these disorders
should be referred to an ophthalmologist.
The episclera lies beneath the conjunctiva and over the sclera. Episcleritis (Fig. 6), which occurs
much less often than conjunctivitis, is a self-limited, recurrent, presumably autoimmune inflammation of the
episcleral vessels. It is
characterized by the rapid onset of redness, a dull ache, and tenderness on palpation. Vision is
unaffected. Discharge, if present, is watery. There are focal areas of redness present within which white sclera may
be observed between radially coursing, dilated episcleral vessels. An oral nonsteroidal antiinflammatory drug (e.g.,
aspirin) may relieve the symptoms, but reassurance that the condition is self-limited and will clear spontaneously
is often all that is required. Persistent or recurrent disease warrants a referral to an ophthalmologist.
Scleritis can impair vision and may be associated with a life-threatening vascular or
connective-tissue disease (e.g., rheumatoid arthritis).33 Fortunately, scleritis is much less common than
conjunctivitis or episcleritis. The redness may be focal or diffuse, and the underlying sclera is pink. Typically,
there is moderate-to-severe, deep ocular pain and tenderness on palpation. The diagnosis of scleritis calls for a
prompt referral to an ophthalmologist; an oral nonsteroidal antiinflammatory drug may help relieve symptoms in the
interim. Treatment often requires systemic corticosteroids, antimetabolites, or both and should be managed
concurrently by the ophthalmologist and the primary care physician.
A pterygium (Fig. 7) is a benign, degenerative conjunctival lesion often seen in hot, dusty
climates, particularly among persons who spend large amounts of time outdoors and are exposed to ultraviolet light
(e.g., fishermen and farmers). A pterygium usually develops over a period of years and is asymptomatic, but the
disorder may be manifested as acute redness of the eye if the lesion becomes inflamed and irritable. The redness is
confined largely to a raised, yellowish,

fleshy lesion that is usually located on the nasal side of the bulbar conjunctiva. The lesion may
extend into the peripheral cornea, but unless the para-central cornea is involved, vision is unaffected. Lubrication
with artificial tears often provides adequate relief. A referral to an ophthalmologist is indicated if the lesion
has recently become larger or has invaded the cornea.
A narrow anterior-chamber angle may occur in persons with hyperopia (farsightedness), because the
globe has a shortened axial length, and in older persons, because the increasing anterior-posterior dimension of the
crystalline lens may push the iris forward.34,35 Signs and symptoms of acute angle-closure glaucoma (Fig.
8) often occur in the evening, when reduced ambient illumination provokes mydriasis, causing the accordion-like
folds of the peripheral iris to block the narrow angle and prevent the outflow of aqueous humor. The result is a
rapid, pronounced elevation of intraocular pressure, with redness of the eye and moderate-to-severe pain. Gentle
palpation through closed lids often confirms that the involved eye is much harder than the uninvolved eye. The
redness is most pronounced in the area adjacent to the limbus (circumcorneal injection). The source of the pain may
not be evident. There have been cases in which nausea and vomiting, associated with headache, were so severe and
persistent that exploratory laparotomy was performed before the importance of the red eye was
recognized.36
In most instances, acute angle-closure glaucoma is unilateral. The pupil of the involved eye is
moderately dilated (i.e., to a diameter of 4 to 6 mm) and unreactive to light; the other pupil is normal. Corneal
haziness, due to edema, causes the iris markings to appear less sharp than those of the uninvolved eye, blurs
vision, and accounts for the classic symptom of seeing haloes around lights. This condition constitutes an ocular
emergency. Optic-nerve atrophy and irreversible loss of vision can occur within hours after the onset of the
disorder. A prompt transfer of care to an ophthalmologist is essential.
Inflammation of the iris and ciliary body, the anterior portion of the uveal tract, usually occurs
in young or middle-aged persons. The hallmark of acute anterior uveitis, also called iritis or iridocyclitis
(Fig.9), is the presence of inflammatory cells and proteinaceous flare in the anterior chamber of one eye. These
features usually cannot be detected without a slit lamp. If the inflammation is severe, however, leukocytes in the
anterior chamber settle and form a hypopyon, a white or yellowish white, flat-topped accumulation of purulent
material that is generally visible without magnification. Symptoms include pain (often characterized as an ache),
photophobia, and blurred vision in the involved eye. Typically, hyperemia is most pronounced in the area adjacent to
the limbus (circumcorneal injection). Discharge, if present, is minimal and watery. Whereas the pupil is semidilated
in angle-closure glaucoma, in anterior uveitis the pupil is constricted and is smaller than that of the unaffected
eye; it may be irregular and, at best, is sluggishly reactive to light. Anterior uveitis can cause glaucoma,
pupillary abnormalities, cataract formation, and macular dysfunction. Since the disorder can impair vision, an
immediate referral to an ophthalmologist is warranted.
A wide variety of factors, including dry eyes, topical medications, viral conjunctivitis, exposure
to ultraviolet light, use of contact lenses, blepharitis, and eyelid abnormalities, can cause superficial keratitis.
This disorder is characterized by an inflammation of the corneal epithelium and superficial stroma, with
conjunctival hyperemia. Multiple punctate lesions - some consisting of nonopaque, microscopic epithelial erosions
that stain strongly with fluorescein dye and others consisting of tiny gray spots - may impart a hazy appearance to
the cornea, impair vision, and cause discomfort. The specific diagnosis and management of this disorder require a
slit lamp and are best left to the ophthalmologist.
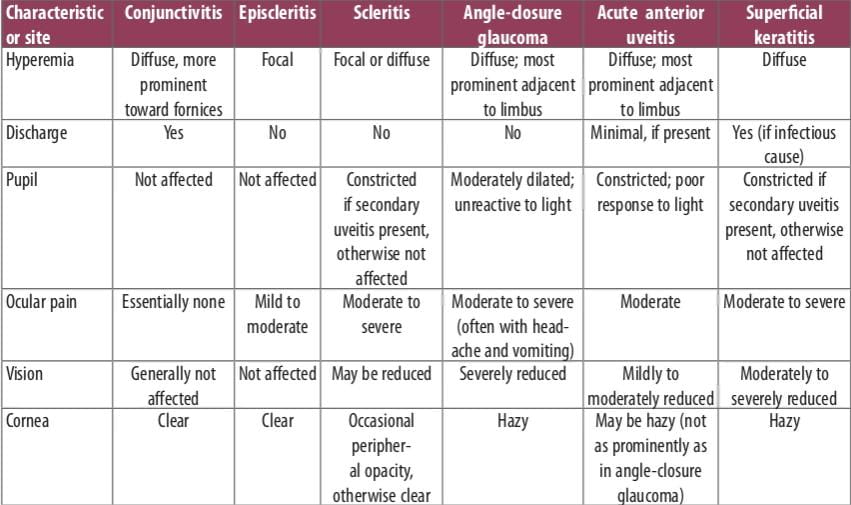
In most cases, the primary care physician can correctly diagnose acute redness of the eye (Table 1)
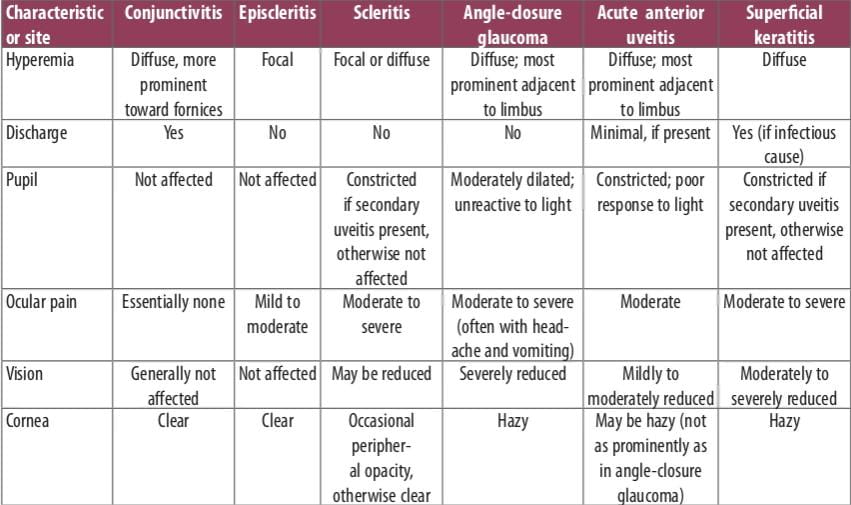
and provide appropriate treatment or refer the patient to an ophthalmologist.If the condition is
chronic or if it recurs frequently, however, the probability that the primary care physician can handle the problem
decreases substantially, and a referral to an ophthalmologist for diagnosis and treatment should be considered.
The following guidelines are invaluable in diagnosing and managing conditions that cause a red eye. A unilateral
red eye associated with vomiting should be considered as acute angle-closure glaucoma until proved otherwise.
Viral conjunctivitis can be highly contagious, and physicians must take great care not to transmit the disease
to themselves or to other patients. A topical corticosteroid or a topical anesthetic should never be prescribed.
Corneal staining with fluorescein and any alteration of corneal transparency merit ophthalmologic consultation.
Severe ocular pain or a visual deficit in association with a red eye calls for immediate intervention by an
ophthalmologist, as does a corneal infiltrate or a hypopyon. In such cases, the primary care physician should
not simply recommend that the patient see an ophthalmologist but should instead transfer the patient to an
ophthalmologist's care immediately.
1. Shapiro MB, Croasdale CR. The red eye: a clinical guide to a rapid and accurate diagnosis.
In: Krachmer JH, Mannis MJ, Holland EJ, eds. Cornea. St. Louis:Mosby, 1997:438-45.
2. Dart JKG. Eye disease at a community health centre. BMJ 1986;293: 1477-80.
3. McDonnell PJ. How do general practitioners manage eye disease in the community? Br J Ophthalmol
1988;72:733-6.
4. McCormick A, Flemming D, Charlton J. Morbidity statistics from general practice: fourth national study
1991-2. London: Her Majesty-s Stationery Office,1995.
5. Manners T. Managing eye conditions in general practice. BMJ 1997; 315:816-7.
6. Leibowitz HM, Pratt MV, Flagstad IJ, Berrospi AR, Kundsin R. Human conjunctivitis. II. Treatment. Arch
Ophthalmol 1976;94:1752-6.
7. Ward JB, Siojo LG, Waller SG. A prospective, masked clinical trial of trifluridine, dexamethasone, and
artificial tears in the treatment of epidemic keratoconjunctivitis. Cornea 1993;12:216-21.
8. Roba LA, Kowalski RP, Romanowski E, et al. How long are patients with epidemic keratoconjunctivitis
infectious? Invest Ophthalmol Vis Sci 1993;34:848.abstract.
9. Nauheim RC, Romanowski EG, Araullo-Cruz T, et al. Prolonged recoverability of desiccated adenovirus type 19
from various surfaces. Ophthalmology 1990;97:1450-3.
10. Leibowitz HM. Antibacterial effectiveness of ciprofloxacin 0.3% ophthalmic solution in the treatment of
bacterial conjunctivitis. Am J Ophthalmol 1991;112:Suppl:29S-33S.
11. Gigliotti F, Hendley JO, Morgan J, Michaels R, Dickens M, Lohr J. Effectiveness of topical antibiotic
therapy in acute conjunctivitis in children. J Pediatr 1984;104:623-6.
12. Miller IM, Wittreich J, Vogel R, Cook TJ. The safety and efficacy of topical norfloxacin compared with
placebo in the treatment of acute, bacterial conjunctivitis. Eur J Ophthalmol 1992;2:58-66.
13. Wilson A. The red eye: a general practice survey. J R Coll Gen Pract 1987;37:62-4.
14. Kulshrestha M, Titcomb L. Topical antimicrobials: role in ocular infections. Prescriber 1998;8:35-40.
15. Prescription Pricing Authority. Electronic PACT data for Kensington, Chelsea and Westminster January-June
1998. Newcastle, England: Kensington, Chelsea and Westminster Health Authority, 1998.
16. Doona M, Walsh JB. Use of chloramphenicol as topical eye medication: time to cry halt? BMJ
1995;310:1217-8.
17. Fraunfelder FT, Bagby GC Jr, Kelly DJ. Fatal aplastic anemia following topical administration of ophthalmic
chloramphenicol. Am J Ophthalmol 1982;93:356-60.
18. Fraunfelder FT, Morgan RL, Yunis AA. Blood dyscrasias and topical ophthalmic chloramphenicol. Am J
Ophthalmol 1993;115:812-3.
19. Donahue SP, Khoury JM, Kowalski RP. Common ocular infections: a prescriber-s guide. Drugs
1996;52:526-40.
20. Albert DM, Jakobiec FA, eds. Principles and practice of ophthalmology: clinical practice. Vol. 4.
Philadelphia: W.B. Saunders, 1994:2828.
21. Soukasian SH, Baum J. Bacterial conjunctivitis. In: Krachmer JH, Mannis MJ, Holland EJ, eds. Cornea. St.
Louis: Mosby, 1997:759-66.
22. Haimovici R, Roussel TJ. Treatment of gonococcal conjunctivitis with single-dose intramuscular ceftriaxone.
Am J Ophthalmol 1989;107:511-4.
23. Dawson CR, Mbekeani JN. Chlamydial infections of the eye. In: Leibowitz HM, Waring GO III, eds. Corneal
disorders: clinical diagnosis and management. 2nd ed. Philadelphia: W.B. Saunders, 1998:644-61.
24. Schachter J. Why we need a program for the control of Chlamydia trachomatis. N Engl J Med
1989;320:802-4.
25. Kline AH, Blettner RJ, Lunin M. Transplacental effect of tetracyclines on teeth. JAMA 1964;188:178-80.
26. Weyman J. The clinical appearances of tetracycline staining on the teeth. Br Dent J 1965;118:289-93.
27. Friedlaender MH. Conjunctivitis of allergic origin: clinical presentation and differential diagnosis. Surv
Ophthalmol 1993;38:Suppl:105-14.
28. Soparkar CN, Wilhelmus KR, Koch DD, Wallace GW, Jones DB. Acute and chronic conjunctivitis due to
over-the-counter ophthalmic decongestants. Arch Ophthalmol 1997;115:34-8.
29. Shine WE, McCulley JP. Meibomian gland triglyceride fatty acid differences in chronic blepharitis. Cornea
1996;15:320-46.
30. McCulley JP, Shine WE. Meibomian gland secretions in chronic blepharitis. Adv Exp Med Biol
1998;438:319-26.
31. Mathers WD, Lane JA, Zimmerman MB. Assessment of the tear film with tandem scanning confocal microscopy.
Cornea 1997;16:162-8.
32. Mathers WD, Lane JA. Meibomian gland lipids, evaporation, and tear film stability. Adv Exp Med Biol
1998;438:349-60.
33. Foster CS, Forstot SL, Wilson LA. Mortality rate in rheumatoid arthritis patients developing necrotizing
scleritis or peripheral ulcerative keratitis: effects of systemic immunosuppression. Ophthalmology 1984;91:
1253-63.
34. Lowe RF. Aetiology of the anatomical basis for primary angle-closure glaucoma: biometrical comparisons
between normal eyes and eyes with primary angle-closure glaucoma. Br J Ophthalmol 1970;54:161-9.
35. Tomlinson A, Leighton DA. Ocular dimension in the heredity of angle-closure glaucoma. Br J Ophthalmol
1973;57:475-86.
36. Ritch R, Shields MB, Krupin T, eds. The glaucomas. Vol. 2. St. Louis: C.V. Mosby, 1989:841.